|
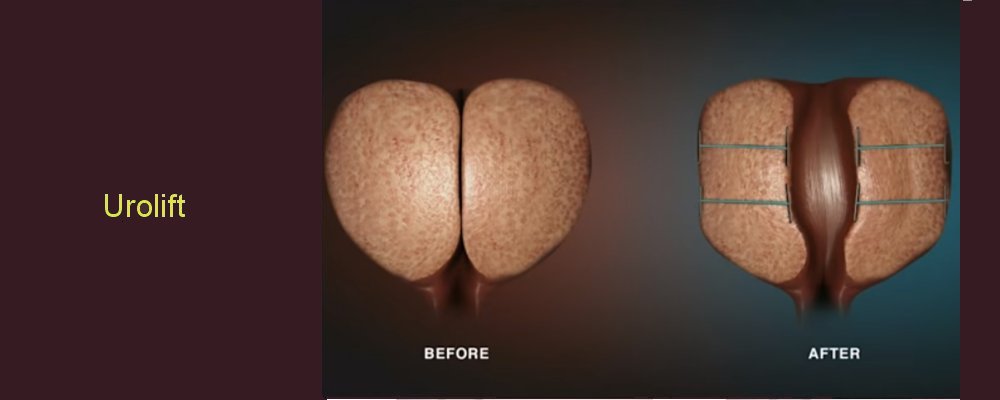
The Urolift device is the very latest non-invasive approach to treating symptomatic BPH. The device lifts or holds the enlarged prostate tissue out of the way so that it no longer blocks the urethra. There is no cutting, heating or removal of prostate tissue. Clinical data has shown that the UroLift System is safe and effective in relieving lower urinary tract symptoms due to BPH.
The major advantages of the PUL using the Urolift device are:
• It does not compromise sexual function – complete maintenance of normal ejaculation and sensation on ejaculation as well as no deterioration of erectile function
• It works immediately; no 3 month delay as with standard surgery – patients often describing improvements in 1 – 3 weeks
•A general anaesthetic may be avoided – a procedure under local anaesthetic alone is increasingly common
• Typically no urinary catheter is required
•Rapid discharge from hospital within hours of the procedure
•A rapid return to normal activities including work in days rather than weeks and months as may be the case after standard surgery.
What does this procedure involve?
-
Your prostate gland sits around your urethra (waterpipe) as it leaves the bladder and, when it enlarges, it can block the flow of urine.
The Urolift procedure involves passing implants into your prostate, using a telescope passed into your bladder. The implants are placed between the inner and outer surfaces of the prostate, so that they pull the obstructing prostate lobes away from your urethra. They become incorporated into the prostate tissue within three months, so they cannot be seen in your bladder after that.
Your urologist can tell you whether the size and shape of your prostate means that this procedure is suitable for you, but it cannot be used in all men with prostate enlargement.
What happens on the day of the procedure?
Your urologist will briefly review your history and medications, and will discuss the surgery again with you to confirm your consent.
An anaesthetist will see you to discuss the anaesthetic options in case this needed as the procedure is usually performed under local anaesthesia and sedation. The anaesthetist will also discuss pain relief after the procedure with you.
We may provide you with a pair of TED stockings to wear, and give you a heparin injection to thin your blood. These help to prevent blood clots from developing and passing into your lungs. Your medical team will decide whether you need to continue these after you go home.
Details of the procedure
We carry out the procedure either under a general or local anaesthetic, according to individual circumstances.
We usually give you an injection of antibiotics before the procedure, after you have been checked for any allergies.
A telescope is then inserted in to your bladder through the urethra.
We put two to four implants into your prostate through the telescope, under direct vision, using a special applicator.
We do not usually need to put a catheter in your bladder at the end of the procedure (which takes 10 to 15 minutes to complete)
Are there any after effects?
The possible after-effects and your risk of getting them are shown below. Some are self-limiting or reversible, but others are not. We have not listed very rare after-effects (occurring in less than 1 in 250 patients) individually.
Temporary burning and stinging when you pass urine (which may last for 5 to 7 days) 1 in 3 patients (34%)
Temporary bleeding in your urine (which may last 5 to 7 days) 1 in 4 patients (26%)
Pain or discomfort in your pelvic area Between 1 in 5 & 1 in 6 patients (18%)
Treatment may not relieve all your symptoms, so that you require further treatment within 5 years Between 1 in 7 & 1 in 8 patients (13%)
Urgency (a sudden need to pass urine with very little warning) 1 in 12 patients (7%)
Temporary urge incontinence (leakage associated with an uncontrollable need to pass urine) 1 in 25 patients (4%)
Inability to pass urine (retention) requiring a short-term catheter in your bladder immediately after the procedure Between 1 in 20 & 1 in 35 patients (3 to 5%)
Infection in your urine requiring treatment with antibiotics Between 1 in 30 & 1 in 35 patients (3%)
Encrustation (stone formation) on the implant(s) requiring later removal Less than 1 in 100 patients (< 1%)
Anaesthetic or cardiovascular problems possibly requiring intensive care (including chest infection, pulmonary embolus, stroke, deep vein thrombosis, heart attack and death) Between 1 in 50 & 1 in 250 patients (your anaesthetist can estimate your individual risk)
What can I expect when I get home?
• You will be discharged when you have passed urine satisfactorily (usually on the same day as your procedure)
• You will get a little burning and bleeding when you pass urine over the first few days
-
• Most men will get some pelvic discomfort for a few days which can be relieved by simple painkillers such as paracetamol
-
• If you are unable to pass urine after the procedure, we may need to put a temporary catheter into your bladder for a few days
-
• If you do need a catheter, we will show you how to manage it at home and will arrange for its removal.
• You will be given a copy of your discharge summary and a copy will also be sent to your GP.
-
• Any antibiotics or other tablets you may need will be arranged & dispensed from the hospital pharmacy.
|