Prostate Cancer Treatment |
||
What additional tests or scans are necessary now I have prostate cancer?
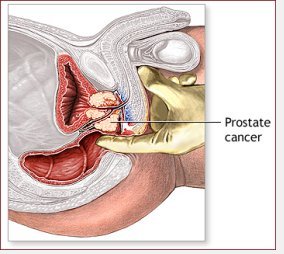
These tests relate mostly to determining if the cancer is confined to the prostate and what chance there is that treatment will fail after a few years. It is possible to combine the information to calculate whether the cancer has spread outside or the chance that the cancer will return after treatment. The information required is: • PSA • Gleason Score • Clinical stage determined by examination of the prostate by a finger • The proportion of positive biopsies
Other investigations, such as magnetic resonance imaging (MRI) can help tell if the cancer is has spread outside the prostate and give information about your anatomy relevant to treatment and side-effects. For this test, you enter a scanning machine, which makes a lot of noise, and produces high quality images of the prostate. It may help determe if the lymph nodes ('lymph glands') contain cancer or not. Sometimes, lymphotropic superparagmagnetic particles are used (this is still under trial). The best way to tell is by laparoscopic lymph node sampling, which is a keyhole procedure for obtaining tissue to examine under the microscope. This is a highly specific test for the identification of cancer in the lymph nodes.
Depending on your individual situation you might choose • Active monitoring • Radical radiotherapy (external beam) • Radical prostatectomy (either open, laparoscopic or robotic) • Brachytherapy • Cryotherapy • High intensity focused ultrasound (HIFU) • Hormone therapy
The situation is often difficult and experts frequently disagree. A careful decision needs to be made usually in conjunction with consultants in radiotherapy and urology.
Part of the problem is that early prostate cancer grows slowly and so treatments are for problems that will often not present for several years. Having said that, the opportunity for curative treatment is available only when cancer is confined to the prostate and has not spread elsewhere.
The prostate cancer is monitored to determine whether it is progressing or not. The implication is that if the prostate appears to be growing and is at risk of causing problems, then a treatment option will be undertaken. To do this, the tumour should be of loss risk of progression anyway. There are no universally accepted criteria for this and a discussion is necessary with an experienced prostate cancer doctor. In patients less than 70 years of age in good health, few doctors would recommend active monitoring especially if the cancer was detected because of urinary symptoms, the Gleason score was 7 or more, or if the PSA was 15 ng/ml or more, or if both sides of the prostate contained cancer (stage T2b or higher). If these conditions do not apply, then active monitoring may be appropriate.
Active monitoring involves regularly measuring the PSA and seeing how it changes. Some people perform prostate examinations regularly and repeat prostate biopsies annually. The idea is to look for evidence that the disease is advancing. Provided it does not advance too far, curative treatment might still be possible or not be necessary! This is becoming a more acceptable way to manage people with prostate cancer. Probably the best strategy is to incorporate all pieces of information regarding the disease and your overall health.
It is possible to calculate the rate at which PSA changes. The faster the PSA increases, the more likely it will be a problem. More than 2 ng/ml in the year per year is thought to be serious. The slower the PSA doubles, the less likely the tumour will affect the individual with it. Conversely, the faster the PSA doubles, the more likely the prostate cancer will cause problems. Men with low grade cancer rarely develop problems until the PSA is greater than 50 ng/ml. If the cancer is high grade, a long or slow PSA doubling time is unreliable although a short doubling time indicates treatment is probably necessary.
The advantage of this option is that the prostate is preserved and the side-effects of treatment are avoided. The disadvantages are that the opportunity for curative treatment might be missed and that our ability to make an accurate estimate of whether a cancer is 'safe' or not is not reliable enough on an individual person basis.
What is a radical prostatectomy?
A radical prostatectomy is the operation to remove the prostate. At the same time the seminal vesicles, which are attached to the prostate, are removed occasionally with the lymph nodes, which are specialised tissue to which the prostate drains. This procedure can be performed by an incision through the lower belly or by key hole techniques ('laparoscopic' or 'endoscopic' or 'robotic'). The advantages are: • The prostate gland with its cancer and surrounding tissue is removed offering what many doctors believe to be the best chance of preserving length of life. This is believed to be most accurate when the cancer is detected because of 'prostate' (urinary) symptoms, the cancer can be felt with a finger, or the cancer is Gleason score 7 or more. • The prostate can be examined completely and a more accurate prediction made of the likley outcome • The PSA should fall to almost unrecordable values making it much easier to determine if the disease has unfortunately recurred • Additional treatment such as radiotherapy can be given with fewer side-effects • Ashort hospital stay (3 to 7 days) is necessary rather than regular attendance • Urinary symptoms (weak or slow flow etc) due to the prostate are usually eliminated completely
The disadvantages are • It is a major operation • A blood transfusion may occasionally be necessary • Control of urine is less good in some after surgery and pads may be required. About 1 in 20 men have problems with leakage and it is more common in men over 70 years of age • Erections may be weaker or non existent although good sexual activity can be had with Viagra, Cialis or Levitra • Additional treatments may be required if the prostate cancer returns
There is strong evidence that radical prostatectomy reduces the chance of dying from prostate cancer by about 50% compared to watchful waiting and deferred androgen deprivation. The evidence comes from a randomised study published in one of the world's most prestigious medical journals. However, the results are most applicable to men with cancer detected because of symptoms, with a PSA around 12 ng/ml, prostate cancer that can be felt with a finger when examined, and Gleason score 6 or 7. Nowadays, many men have few urinary symptoms, PSA values around 5 to 8, Gleason score 6 and impalpable cancer ie the cancers are detected earlier in their history. This is not to say that surgery is not effective just that to benefit one has to wait longer.
The procedure can be performed through a traditional incision in the lower abdomen or through 5 very small incisions ie endoscopic or laparoscopic surgery. The advantages of laparoscopic surgery include improved view allowing more precise surgery, shorter hospital stay (2-3 days) and earlier return to leisure activities and work. It is technically difficult to and specialised training is required.
Robotic prostate surgery Laparoscopic prostatectomy da Vinci Surgical System
The prostate is treated by radiotherapy given whilst lying in a machine at a special hospital. Usually, one attends on week days for 6 to 7 weeks for a short time for the treatment. This treatment is sometimes accompanied or preceded by hormonal therapy to block the effects of testosterone, which is the male hormone that drives prostate growth. The advantages are: • The prostate cancer is treated and is less likely to recur or cause symptoms • There is a much lesser chance of incontinence compared to radical prostatectomy or brachytherapy, but frequency or urgency may be worse • Radiotherapy can be given to the side walls of the pelvis which may be important if the cancer has spread. • HIFU or cryotherapy can be used if radiotherapy fails • Surgery is avoided
There are disadvantages too: • Many doctors believe that radiotherapy is probably a less effective treatment than surgery when compared over long periods of follow up • Side-effects include diarrhoea, and blood in the stools • Erections become weaker over time • It is more difficult to use the PSA to determine if the treatment has been successful or not • If treatment fails, cryotherapy or surgery is associated with more side-effects such as worse incontinence
Seeds with radiotherapy energy are placed systematically in the prostate under a general anaesthetic. Patients stay in hospital usually overnight. This is done either in one or two stages depending on the set up.
The advantages are: • This can be a day case procedure so patients can often leave the same day • It is possible to have additional therapy, usually external beam therapy, if there is disease recurrence • Incontinence of urine is less likely
The disadvantages include • Urinary symptoms often become significantly worse after surgery and sometimes a catheter is required for a period to empty the bladder • The treatment is probably less effective than surgery regarding cancer cure • Weakness of erections occurs, although possibly less commonly than after surgery or external beam radiotherapy
The prostate and its cancer can be killed by freezing the cells. To give this therapy, a general anaesthetic is necessary and a catheter needs to be placed for several days.
The main advantage is that it can be given after radiotherapy if it is not effective. It can also be repeated. However, it almost always causes erectile dysfunction. Expertise with its use is limited in the UK.
This usually refers to reducing testosterone levels in the body and is usually known as androgen deprivation, androgen suppression or castration. Testosterone with its derivative dihydrotestosterone is the male hormone that drives prostate growth. Rather than reduce the levels of testosterone, its action can be blocked by drugs and this is known as androgen blockade.
This form of therapy is usually used with or without radical radiotherapy, and sometimes after radical surgery but not before. The prostate cancer tends to be more advanced than early.
The side effects of this include hot flushes, tiredness, anaemia, and in the long term osteoporosis.
What is HIFU?
High Intensity Focused Ultrasound (HIFU) is the name for a technique to treat prostate cancer. Like a magnifying glass focuses light rays to a focal point, HIFU concentrates sound waves on a precisely targeted, tiny area of diseased tissue. HIFU heats the tissue to about 100°C degrees and destroys it. The advantage of visually Directed HIFU over conventional HIFU is that the surgeon uses real-time feedback to adjust the amount of energy needed to ensure eradication of the diseased tissue whilst protecting healthy tissues. The active involvement of the surgeon in the planning and treatment achieves a higher rate of success. HIFU is a relatively new treatment that has become popular as it is minimally invasive with few side effects.
You have to trade-off the advantages over the disadvantages of each option. It depends on the relative values of each. This is best done by discussing the issues with a doctor and close family. In general, if the thought of having cancer and not doing the most possible to get rid of it dominates your thinking, then you should choose an interventional treatment. There is no caste iron evidence to indicate one treatment is better than another, but many doctors believe that radical prostatectomy offers the best chance of prolonging life. It becomes more important to maximally remove the cancer if it is high risk or there are many years of life possibly ahead. On the other hand, active monitoring may be the best option if quality of life is more important than preserving a few years of life especially if there is uncertainty over the benefit of treatment and the cancer does not seem obviously to be high risk. A second opinion is often helpful.
Several websites offer details and on-line help in making decisions including:
Prostate Cancer UK (link) | ||
|
|
Summary |
|
